Abstract
Objectives Infection remains a major cause of morbidity and mortality after hematopoietic stem cell transplant (HSCT). With recent changes in transplant practices, such as the increasing use of alternative donors and T-cell depletion, how various risk factors interplay and affect the timeline of infections have not been well elucidated in children. While the epidemiology and risk factors for viral infections post-HSCT were well described for cytomegalovirus (CMV) and Epstein-Barr virus (EBV), the corresponding information on human herpes virus 6 (HHV-6), adenovirus (ADV) and BK virus (BKV) infection in children is limited. This study aims to review comprehensively the epidemiology, risk factors and outcome of bacterial, viral and fungal infections after contemporary HSCT to inform future infection prophylaxis strategies.
Method We retrospectively reviewed the first 100 consecutive HSCT for malignant and non-malignant diseases from April 2019 to October 2021 in the only pediatric HSCT center in Hong Kong. The incidences were recorded and risk factors were analyzed for bacterial, viral and fungal infections and infection-related mortality.
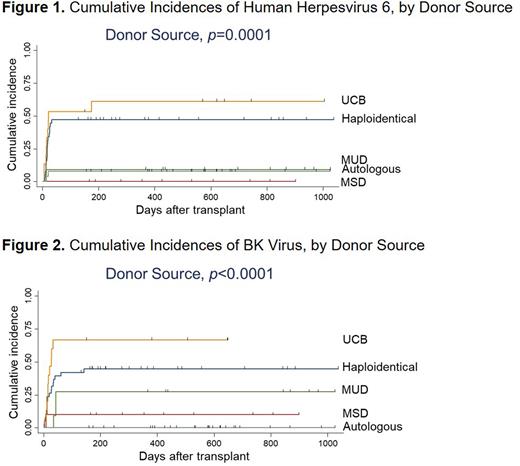
Results The vast majority of the allogeneic transplant recipients (69/74, 93.2%) had infections after HSCT, amongst which bacterial, viral and fungal infection rate was 35.1%, 90.5% and 9.5% respectively. In contrast, only 30.8% (8/26) of autologous transplant recipients had infections, and their respective rate of bacterial, viral and fungal infection was 19.2%, 15.4% and 3.8%. HHV-6 and BKV typically occurred early after HSCT, ADV and varicella zoster virus (VZV) thereafter, and CMV and EBV throughout the entire 2.5-year observation period. The cumulative incidences of HHV-6 and BKV were significantly higher in patients receiving umbilical cord blood (UCB) or haploidentical stem cell transplant (p = 0.0001; p <0.0001, respectively) when compared with matched sibling (MSD) or matched unrelated donor (MUD) transplant (Figure 1 and 2). Ex vivo T-cell depletion was a general risk factor for viral infection with HHV-6 (HR = 3.03), BKV (HR = 3.36), CMV (HR = 4.45) and EBV (HR = 7.15); all p < 0.02. Cancer in second- compared with first-complete remission was a risk factor for bacterial infection in multivariate analyses (OR = 6.0, 95% CI = 1.12-32.2, p = 0.037). Patients with gut graft-versus-host disease were at risk for fungal infections (OR = 12.3, 95% CI = 1.33-114.4, p = 0.027). The infection-related mortality (IRM) rate was 10%, which occurred only in allogeneic HSCT patients with hematological malignancies receiving cord blood (n = 4) or haploidentical HSCT (n = 6). History of bacterial infection after HSCT was associated with an increased risk of IRM (HR = 4.13, 95% CI = 1.05-16.3, p = 0.042).
Conclusion Not all HSCT recipients are of equal risk to infections and IRM. Our findings in pediatric patients after contemporary HSCT support both time-dependent and risk-adapted measures against infective complications to improve transplant outcome.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal